A key focus for I-TECH in Ukraine is strengthening the capacity of local partners to develop and deliver high-quality clinical trainings and expand the supply of skilled health care workers.
Category: HIV Care and Treatment
Nancy Puttkammer

Nancy Puttkammer is an Acting Assistant Professor within the Department of Global Health at University of Washington and is the faculty co-lead of the Digital Initiatives Group at I-TECH (DIGI). Her interests are in strengthening health information systems and promoting data use and for quality improvement of health programs in resource-limited settings. She is trained as a health services researcher, specializing in using observational, routinely-collected data from electronic medical records (EMRs) to strengthen HIV care and treatment programs.
In her capacity as a Research and Evaluation Advisor at the International Training and Education Center for Health, Dr. Puttkammer works with informatics and training projects in Haiti, Kenya, and South Africa to improve large-scale implementation of EMRs, evaluate data quality and data use, support data analyses, and develop capacity for data use and implementation science research among colleagues and counterparts. Dr. Puttkammer has a PhD in Health Services from the University of Washington and an MPH in Community Health Education from the University of California, Berkeley.
Program Highlights
Scott Barnhart
Scott Barnhart, MD, MPH, has an extensive background as Professor of Global Health and former Director of Global Health Programs for I-TECH at the University of Washington. He has had responsibility for leading nine country offices, projects in 14 countries, and more than 500 staff. This experience and training has included extensive clinical work, research and program management in pulmonary and environmental and occupational medicine, and more than eight years as Medical Director of a safety net/Level 1 Trauma Center hospital.
Ensuring health systems can quickly detect and respond to emerging health threats is a critical challenge in both domestic and global health. Dr. Barnhart’s major implementation projects include scale-up of voluntary medical male circumcision (VMMC) in Zimbabwe and Malawi, OpenMRS, and laboratory information systems. Dr. Barnhart deploys his expertise in multiple African countries and Haiti to strengthen health systems and health care.
A goal of Dr. Barnhart’s work is to promote country-led, country owned sustainable development. Consistent with the principles of the Paris Declaration, the goal is to transition the bulk of development work and the associated leadership, ownership, technical direction and control of funding into the countries where development occurs. This approach ensures that the entire continuum of skills necessary for development (technical expertise, administration (human resources, operations, and management and accountability for funds) is transitioned to local partners. A key indicator is to have 75% or more of a grant’s funding expended in-country on local programs and local citizens and to support the local economies in these highly resourced constrained countries. Dr. Barnhart has worked closely to advance this model through projects in Haiti with a goal to shift the majority of a project to a local organization and in Zimbabwe where the VMMC program is largely run through local partners.
Program Highlights
Health Information Systems in Haiti
Electronic medical record (EMR) systems have the capacity to improve clinical decision making and quality of care at site level but can also be leveraged to make data-driven, population-level public health decisions. At the request of the MSPP Continue reading “Health Information Systems in Haiti”
Clinical Mentoring in Haiti
I-TECH introduced its clinical mentoring program in Haiti in 2006. A team of physicians, nurses, and psychologists provide technical assistance to 20 sites in the MSPP care and services network to help strengthen HIV- and AIDS-related services. During site visits, CHARESS mentors conduct clinical rounds Continue reading “Clinical Mentoring in Haiti”
I-TECH Ukraine Conducts ARVs for Epidemic Control Workshop

In early April, the International Training and Education Center for Health (I-TECH) conducted a five-day workshop on “Antiretroviral Drugs for Epidemic Control” for more than 50 chief doctors and deputy chief doctors from Regional AIDS Centers in Ukraine.
Workshop participants learned about evidence-based, international best clinical practices and the cost-effectiveness of strategies for using antiretroviral therapy (ART) to control HIV epidemics. International keynote speakers included:
- Dr. Jeremy Penner, International Clinical Advisor in Ukraine to I-TECH/University of Washington (UW);
- Dr. Elliot Marseille, Consultant to I-TECH/UW and the Center for Global Surgical Studies at the University of California, San Francisco;
- Dr. Michael Martin, U.S. Centers for Disease Control and Prevention (CDC) Senior Technical Advisor for HIV/AIDS care and treatment in Thailand; and
- Dr. Juliana de Fatima da Silva, Epidemic Intelligence Service Officer at the CDC.
The pool of facilitators also included nine national experts from the Ministry of Health’s Center of Public Health (CPH).
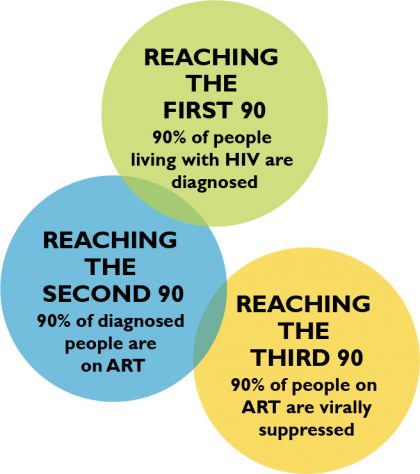 The workshop aimed to support the development of efficient strategies to achieve the UNAIDS 90-90-90 goals: 90% of HIV-positive people know their status, 90% of those are on treatment, and 90% of those are virally suppressed. To this end, the workshop covered national situational analysis, national clinical recommendations, and service delivery models with the highest potential for adaption in country.
The workshop aimed to support the development of efficient strategies to achieve the UNAIDS 90-90-90 goals: 90% of HIV-positive people know their status, 90% of those are on treatment, and 90% of those are virally suppressed. To this end, the workshop covered national situational analysis, national clinical recommendations, and service delivery models with the highest potential for adaption in country.
Progress on ART optimization in Ukraine was shared, and participants were able to discuss their experiences and ideas for improving HIV-related services. The presentations and group discussions were particularly timely, given the development of complex new HIV clinical guidelines currently under way in Ukraine – they also provided much needed evidence to support this process.
Similar workshops were requested by the CPH and leaders of the Regional AIDS Centers, and I-TECH plans to meet this request by conducting two workshops in June and September 2017.
THIS PROJECT IS SUPPORTED BY THE HEALTH RESOURCES AND SERVICES ADMINISTRATION (HRSA) OF THE U.S. DEPARTMENT OF HEALTH AND HUMAN SERVICES (HHS) UNDER U91HA06801, THE INTERNATIONAL AIDS EDUCATION AND TRAINING CENTER (IAETC). THE CONTENT OF THIS POST IS THE AUTHOR’S AND SHOULD NOT BE CONSTRUED AS THE OFFICIAL POSITION OR POLICY OF, NOR SHOULD ANY ENDORSEMENTS BE INFERRED BY HRSA, HHS OR THE U.S. GOVERNMENT.
CUGH 2017: Text Messaging and Tablets for Training

On April 6, the International Training and Education Center for Health (I-TECH) headed to the 8th Annual Consortium of Universities for Global Health (CUGH) Conference in Washington, D.C. I-TECH Zimbabwe presented among many colleagues in the University of Washington’s Department of Global Health, including staff of the department’s E-Learning Program (eDGH), which has worked closely with I-TECH on a number of e-learning and blended learning training programs.
This year’s conference theme was “Healthy People, Healthy Ecosystems: Implementation, Leadership & Sustainability in Global Health,” and I-TECH’s entries highlighted its sustainable workforce development work worldwide.

I-TECH Zimbabwe’s Vivian Bertman shared results on the use of text messaging as a low-cost, sustainable platform for building health care worker skills and knowledge to care for children and adolescents with HIV.
The research, titled “Health Worker Text Messaging for Training Peer Support, and Mentoring in Pediatric and Adolescent HIV/AIDS Care: Lessons Learned in Zimbabwe,” assessed the use of WhatsApp in a blended learning program. Participants used the app for peer-to-peer learning and support, generating over 300 entries, continuing discussions after course completion, and creating spin-off groups, including a support group for teens.
Highlighting the flexibility of cost-effective e-learning approaches was an oral presentation by eDGH’s Leslie Wall and Anya Nartker titled “No internet? No problem! Creative approaches to cost-effective e-learning delivery in resource-constrained settings.” The research looked at five tablet-based training programs developed by eDGH, in partnership with I-TECH, and delivered in Namibia, Tanzania, and Zimbabwe.
For participants, time spent off the job decreased from four days to less than one day, and within training programs that used text messaging to keep learners engaged, all participants finished in the time allotted. The team plans to expand learning activities and incorporate additional real-time interactions via text-message-based discussion groups or added face-to-face interactions.

Caitlin O’Brien-Carelli, an MPH graduate from the UW Global Health program, explored additional sustainable training models. O’Brien-Carelli presented her MPH thesis work on behalf of I-TECH: “Training Healthcare Workers on the Use of Electronic Medical Records in HIV Clinics in Kenya: An Evaluation of Three Training Models.”
During I-TECH Kenya’s first years of training health care workers to use the KenyaEMR system, the team adjusted its training from 5 days to 3 days, and moved the training from off-site to on-site, to increase sustainability and maintain effectiveness. Results confirmed that with the adjustments, training quality was maintained, more people in more facilities were trained, and costs were reduced significantly.
Detailing innovations on the operations front, I-TECH HQ Managing Director Rob Lindsley presented at a conference satellite session titled “Global Operations 2017: Tools for Faculty & Administrative Leaders.” Lindsley’s presentation, “It’s About How Hard You Can Get Hit and Keep Moving Forward: Global Support and PLC Registration in India,” outlined I-TECH’s complicated, creative pathway to country office registration in India.
Ukraine’s HIV/AIDS Clinics Embrace ClASS Approach

This month, the International Training and Education Center for Health (I-TECH), working with the Ministry of Health (MOH) in Ukraine, sensitized heads and other managers of HIV/AIDS clinics and centers on how to implement continuous quality improvement (CQI) by applying an approach known as the Clinical Assessment for Systems Strengthening, or ClASS, model.
The MOH’s Center of Public Health and I-TECH Ukraine held a two-day ClASS sensitization workshop for HIV clinicians from seven regions of Ukraine that are new to ClASS. The ClASS approach addresses CQI and identifies areas for improvement and assessment as well as detailed follow-up actions.
Presentation of the model was supplemented by reports and success stories shared by teams from Cherkasy, Kyiv, Chernivtsi Oblast, and Kryviy Rig City AIDS Centers, along with other sites that participated in ClASS between 2014 and 2016. The exchange of this experience proved effective in ensuring buy-in from new regions and raised their interest in and excitement about the model and its potential impact.

I-TECH Ukraine Program Director Iryna Yuryeva, who presented the ClASS model, said she was encouraged by the response to the workshop. Perceptions among the new audience shifted “amazingly quickly” she said, “from extreme concern, anxiety, and belief that almost nothing can and should be improved at their health care facilities to sincere and passionate interest and impatient anticipation of ClASS visits in the coming months.”
Participants expressed keen interest in the ClASS approach, which emphasizes team problem-solving and joint identification of ways to improve assessment, develop operational and strategic plans, and seek technical assistance when needed to address gaps. In addition, ClASS could also be helpful for health care facilities preparing for formal accreditation by addressing assessment-based practical recommendations.
The “real-life cases and improvements” reported by the participating clinicians, and their ability to exchange experiences and proactively tackle main areas for improvement, were highlights of the training. This is all part of the ClASS methodology, a process that I-TECH’s Yurveya says demonstrates a “natural and evolutionary continuous quality improvement.”
I-TECH Ukraine will continue to support the MOH by promoting the ClASS approach as part of the CQI process in Ukraine, in particular by conducting additional ClASS trainings in seven new regions in 2017.
THIS PROJECT IS SUPPORTED BY THE HEALTH RESOURCES AND SERVICES ADMINISTRATION (HRSA) OF THE U.S. DEPARTMENT OF HEALTH AND HUMAN SERVICES (HHS) UNDER U91HA06801, THE INTERNATIONAL AIDS EDUCATION AND TRAINING CENTER (IAETC). THE CONTENT OF THIS POST IS THE AUTHOR’S AND SHOULD NOT BE CONSTRUED AS THE OFFICIAL POSITION OR POLICY OF, NOR SHOULD ANY ENDORSEMENTS BE INFERRED BY HRSA, HHS OR THE U.S. GOVERNMENT.
Patient-Trainers are Key to Providing High-Quality Care to MSM, Sex Worker, and Transgender Communities in the Caribbean

For many communities in the Caribbean Region, barriers to high-quality HIV treatment and care often arise before a client crosses the clinician’s threshold.
“When [key populations] access health care – and when we say key populations, we mean MSM [men who have sex with men], sex workers, transgender people – they are immediately discriminated against,” says Kenyatta Barnaby, a Key Populations (KP) Advisor working with the International Training and Education Center for Health (I-TECH) in Jamaica.
“They can’t relate to the clinician or anyone in their surroundings,” continues Barnaby, “and before they even get to [see] the clinician, there is discrimination in the waiting area.”
If a patient makes it far enough to see a clinician, the stakes become higher – misunderstandings and miscommunication can have grave consequences. Barnaby notes that, often, clients from key populations are afraid to contradict a clinician’s assumptions and may not share information that’s vital to receiving proper care.
When clients do disclose that they are gay, transgender, or doing sex work, “[a clinician] might express disgust or alarm,” explains Conrad Mitchell, I-TECH’s Key Populations Advisor in Trinidad & Tobago. “What happens directly as a result of that is that someone feels alienated, and therefore does not come back and does not get the care that they need.”
When these experiences are shared within community networks, it can result in fewer people from key population groups accessing care at facilities where others have had negative experiences.

A novel approach using real-world experiences
To address these challenges in HIV care and treatment settings, I-TECH designed and launched Improving HIV Care for Key Populations in the Caribbean, a novel preceptorship program aimed at building clinicians’ capacity to provide nonjudgmental, high-quality, comprehensive HIV care to most-at-risk communities.
The two-day intensive training occurs in a simulated clinic setting, using targeted role-play scenarios based on real-world experiences. “Patients” are portrayed by skilled KP patient-trainers under the supervision of an experienced clinical facilitator. Clinician trainees participate in 8 to 12 different clinical scenarios featuring patients who are transgender, MSM, or doing sex work.
During these trainings, clinicians practice taking a comprehensive sexual history, performing a proper (simulated) ano-genital examination with appropriate site-specific STD screening, conducting rapid mental health screenings, and undertaking individual risk assessment and risk reduction counseling.
The program was developed and implemented by I-TECH in close collaboration with key population groups in in the region. I-TECH developed standardized case scenarios collaboratively with community members, and recruited and trained representatives from the sex worker, MSM, and transgender communities in each country to portray these scenarios as the patient-trainer and to give targeted feedback to clinicians.
Frank, face-to-face discussions
Once the trainer exits the role of “patient,” the clinician is also afforded the opportunity to have a frank and open discussion with the trainer. These conversations are wide-ranging – from the obstacles that prevent key populations from accessing care; to the health care issues they face; to psychosocial issues such as mental health, gender affirmation, gender-based violence, and substance abuse.
“One of the great things that can come out of something like this,” says Mitchell, “is although the person has come in with a physical problem, we are sensitizing the clinician to see past that.”
The patient-trainers share powerful personal stories with the clinicians, noting how small actions or expressions – such as a slight grimace or donning gloves to take blood pressure – can be interpreted as stigma. They offer insight into what runs through a patient’s mind at a health facility: fear of harassment by vendors, security staff, and other patients; anxiety around disclosing they have same-sex partners, the number of partners, or sexual practices; and reluctance to seek care for ano-genital conditions.
The patient-trainers also teach providers about the importance of using preferred names and pronouns, about avoiding the assumption of heterosexuality, and of showing a non-judgmental attitude. “A lot of it is about language,” says Barnaby. “We are equipping them with the knowledge of how to speak to a KP person without discriminating.”

A two-way street
For some clinicians, this training is the first time meeting a transgender person, or the first time receiving constructive feedback about service delivery from the perspective of the patient. Clinicians have noted that they appreciate opportunities to interact with real people from the key population groups and to get feedback on their clinical practice and interpersonal skills directly from a patient’s perspective.
Mitchell, who portrays several patients throughout the training program in Trinidad, also notes that “there is always that ‘wow’ moment with the clinicians: ‘Wow, I didn’t know this was happening.’” Mitchell says that he had a clinician admit to him that the many years of schooling that doctors go through can leave them naïve of social issues.
Perhaps most valuably, the understanding is not one-sided. At the end of the two days, says Mitchell, not only is there a marked improvement in the clinicians, but the patient-trainers come away enlightened, as well.
“Often we forget that doctors are people themselves,” he says. “I think that’s one of the things that the team in Trinidad collectively learned. Because there were a number of doctors that came to the training, and we had sort of a negative view of them…. Often what comes across as negative is this person having a rough day, a bad day, or not being able to give the kind of help they want to give.”
Barnaby echoes that sentiment, noting that a doctor can quickly get a bad reputation within the tight-knit KP communities in Jamaica, and these trainings have helped bridge the gap from both sides. “If the preceptorship trainers can see the doctor’s potential to be good,” says Barnaby, “he gets a good rep in the community, as well.”
So far the program has trained 20 clinicians from the highest volume HIV care and treatment clinics in Jamaica and Trinidad. In the coming year, I-TECH will continue to train clinicians and will also adapt the training for nurses in the region.
THIS PROJECT IS SUPPORTED BY THE HEALTH RESOURCES AND SERVICES ADMINISTRATION (HRSA) OF THE U.S. DEPARTMENT OF HEALTH AND HUMAN SERVICES (HHS) UNDER U91HA06801, THE INTERNATIONAL AIDS EDUCATION AND TRAINING CENTER (IAETC). THE CONTENT OF THIS POST IS THE AUTHOR’S AND SHOULD NOT BE CONSTRUED AS THE OFFICIAL POSITION OR POLICY OF, NOR SHOULD ANY ENDORSEMENTS BE INFERRED BY HRSA, HHS OR THE U.S. GOVERNMENT.
D.C. Study Tour to Inform Continuing Medical Education in Ukraine

Ukraine has the second largest HIV epidemic in eastern and central Europe; an estimated 220,000 citizens were living with the disease as of January 2016. As part of national efforts to help curb the impact and spread of HIV, the Ukrainian government is expanding and scaling up HIV services – training is an integral part of this scale-up.
To this end, the International Training and Education Center for Health (I-TECH) is working with national partners in Ukraine to build local capacity to provide high-quality continuing medical education (CME) on HIV and related topics.
Most recently, I-TECH arranged for representatives from the Ukrainian Center for Socially Dangerous Disease Control (UCDC) of the Ministry of Health and the Ukrainian Family Medicine Training Center, based at Bogomolets National Medical University, to participate in a weeklong study tour in Washington, D.C.
“Participants found the study tour to be extremely informative and timely given reforms to health workforce development currently under way in Ukraine,” said Anna Shapoval, I-TECH Ukraine Country Representative. “The information obtained and contacts established through the study tour will help to inform development of an HIV-focused professional medical association in Ukraine.”
The aim of the association will be to advocate on behalf of medical providers, educate health professionals on new developments in clinical practice and relevant legislation and other issues affecting HIV medicine and patients, and potentially provide crucial CME opportunities.
Tour participants met with representatives from CME training networks, HIV-focused professional medical associations, and organizations involved with CME accreditation and physician licensure in the U.S. Highlights from the tour include:
- Meeting with the U.S. Human Resources and Services Administration (HRSA) on HRSA’s mission and activities, including the AIDS Education Training Center Program and other initiatives to improve HIV services in the U.S.
- Informative sessions with the Maryland State Board of Physicians and Federation of State Medical Boards on the role of state medical boards in physician licensure
- An overview and discussion on CME accreditation requirements and standards for commercial support
- Meetings with various HIV-focused professional medical associations to discuss their establishment, funding models, advocacy work, CME and certification offerings, and lessons learned
The study tour participants identified several aspects of the U.S. CME and licensure systems to explore further and potentially apply in Ukraine, including decentralized licensure, nongovernmental CME accreditation, and diverse CME providers such as universities and professional associations.