A key focus for I-TECH in Ukraine is strengthening the capacity of local partners to develop and deliver high-quality clinical trainings and expand the supply of skilled health care workers.
Category: eLearning/Distance Learning
Nancy Puttkammer

Nancy Puttkammer is an Acting Assistant Professor within the Department of Global Health at University of Washington and is the faculty co-lead of the Digital Initiatives Group at I-TECH (DIGI). Her interests are in strengthening health information systems and promoting data use and for quality improvement of health programs in resource-limited settings. She is trained as a health services researcher, specializing in using observational, routinely-collected data from electronic medical records (EMRs) to strengthen HIV care and treatment programs.
In her capacity as a Research and Evaluation Advisor at the International Training and Education Center for Health, Dr. Puttkammer works with informatics and training projects in Haiti, Kenya, and South Africa to improve large-scale implementation of EMRs, evaluate data quality and data use, support data analyses, and develop capacity for data use and implementation science research among colleagues and counterparts. Dr. Puttkammer has a PhD in Health Services from the University of Washington and an MPH in Community Health Education from the University of California, Berkeley.
Program Highlights
CUGH 2017: Text Messaging and Tablets for Training

On April 6, the International Training and Education Center for Health (I-TECH) headed to the 8th Annual Consortium of Universities for Global Health (CUGH) Conference in Washington, D.C. I-TECH Zimbabwe presented among many colleagues in the University of Washington’s Department of Global Health, including staff of the department’s E-Learning Program (eDGH), which has worked closely with I-TECH on a number of e-learning and blended learning training programs.
This year’s conference theme was “Healthy People, Healthy Ecosystems: Implementation, Leadership & Sustainability in Global Health,” and I-TECH’s entries highlighted its sustainable workforce development work worldwide.

I-TECH Zimbabwe’s Vivian Bertman shared results on the use of text messaging as a low-cost, sustainable platform for building health care worker skills and knowledge to care for children and adolescents with HIV.
The research, titled “Health Worker Text Messaging for Training Peer Support, and Mentoring in Pediatric and Adolescent HIV/AIDS Care: Lessons Learned in Zimbabwe,” assessed the use of WhatsApp in a blended learning program. Participants used the app for peer-to-peer learning and support, generating over 300 entries, continuing discussions after course completion, and creating spin-off groups, including a support group for teens.
Highlighting the flexibility of cost-effective e-learning approaches was an oral presentation by eDGH’s Leslie Wall and Anya Nartker titled “No internet? No problem! Creative approaches to cost-effective e-learning delivery in resource-constrained settings.” The research looked at five tablet-based training programs developed by eDGH, in partnership with I-TECH, and delivered in Namibia, Tanzania, and Zimbabwe.
For participants, time spent off the job decreased from four days to less than one day, and within training programs that used text messaging to keep learners engaged, all participants finished in the time allotted. The team plans to expand learning activities and incorporate additional real-time interactions via text-message-based discussion groups or added face-to-face interactions.

Caitlin O’Brien-Carelli, an MPH graduate from the UW Global Health program, explored additional sustainable training models. O’Brien-Carelli presented her MPH thesis work on behalf of I-TECH: “Training Healthcare Workers on the Use of Electronic Medical Records in HIV Clinics in Kenya: An Evaluation of Three Training Models.”
During I-TECH Kenya’s first years of training health care workers to use the KenyaEMR system, the team adjusted its training from 5 days to 3 days, and moved the training from off-site to on-site, to increase sustainability and maintain effectiveness. Results confirmed that with the adjustments, training quality was maintained, more people in more facilities were trained, and costs were reduced significantly.
Detailing innovations on the operations front, I-TECH HQ Managing Director Rob Lindsley presented at a conference satellite session titled “Global Operations 2017: Tools for Faculty & Administrative Leaders.” Lindsley’s presentation, “It’s About How Hard You Can Get Hit and Keep Moving Forward: Global Support and PLC Registration in India,” outlined I-TECH’s complicated, creative pathway to country office registration in India.
Success Story: WhatsApp, a Potential Warmline for Low-Resource Settings

In Zimbabwe, health care workers often need to build confidence and skills in caring for HIV-positive infants and children. The International Training and Education Center for Health (I-TECH) has employed an innovative approach to support these front-line staff – a case-based, self-study PMTCT Client Retention training.
During the introductory session, participants are oriented to the course, given self-study tips, loaned tablets and instructed on their use, and given a pre-course assessment. Participants also attend a half-day classroom session at the beginning and end of the five-week course.
A WhatsApp discussion group is also set up to send messages of motivation and reminders and for participants to share issues during the course. WhatsApp is widely used in Zimbabwe as an inexpensive mobile phone platform to message individuals and groups.
WhatsApp for collaborative problem solving
Elizabeth is a primary care nurse who was among a cohort of 30 participants in one of these trainings, conducted in Mashonaland Central Province. About one week into the course, Elizabeth faced a situation at work where she was confused about how to apply national guidelines to one of her pediatric patient cases. Elizabeth chose to bring the issue to her training cohort. Below is a sample of the discussion that ensued among several members of the group, showing that a number of the cohort were similarly perplexed:
Elizabeth: A woman came to our clinic. She was ill. She wanted to get tested because she was ill for a long time on and off. The woman tested positive. Because she is breastfeeding an 11-month-old baby l commenced her on Option B+. l tested the baby with antibody RDT [rapid diagnostic test] and tested negative. l commenced the baby on cotrimoxazole prophylaxis. The question is: Was it necessary for the baby to be given NVP [nevirapine] prophylaxis since the baby tested negative and is now 11 months OR should l give the baby NVP prophylaxis for 6wks from now????
Elizabeth received a range of responses from her cohort:
- NVP is only given from birth up to six weeks. Commence mother on Option B+, baby on cotr prophylaxis collect confirmatory DBS [dried blood spots] for the child.
- I agree with ~nr
- Cotr prophylaxis and confirmatory DBS only for the baby. Thanks guys.
- Baby should still get NVP for six wks since still breastfeeding — meaning baby is still exposed.
- As per NVP shld be given — the first dose at birth, the second dose 48hrs after first dose, then third dose 96hrs after second dose. Prophylaxis shld be given as soon after delivery as possible. When prophylaxis is delayed the less likely that the infection will be prevented.
- By age of 14 days, infection already would be established in most infants. So l think it’s not necessary to give NVP as prophylaxis.
One member of the cohort was a district nursing officer (DNO). He shared that he had deliberately delayed responding until others had weighed in. He not only gave advice but also encouraged the group to refresh themselves on the resources available on their tablets:
Sorry for a late response. Remember key things in your scenario: mother is positive, baby is breastfeeding and is 11 months. … Infant is still at risk, therefore cotri prophy, infant feeding counselling and a continuation of routine FCH [family and child health] care will help. Then 6wks after stopping breastfeeding conduct rapid HIV test again. If negative stop cotri prophy and continue routine care. If positive CT cotri prophy, initiate ART.
He then referred Elizabeth to an algorithm in the national ART guidelines, which were included for easy reference in an application on the participants’ tablets.
This exchange showed the potential use of WhatsApp for support in clinical decision making, in the absence of a warmline for consultation. Upon returning to the classroom, participants engaged in discussion around the WhatsApp conversations, with particular attention paid to the case that Elizabeth had brought to the group. Other members of the cohort reported that they had watched the exchange with interest though they did not contribute.
The cohort members reported that the case was educational for them, and many of them indicated that they would like to continue their group for ongoing support.
As for Elizabeth’s young client, a rapid test was collected and returned negative. Results of the DNA test are still being awaited by the group with much interest. As one member wrote: “We cannot afford to lose that child, wherever she is. … She is still our child.”
E-Learning and Data Quality Improvement Featured at CUGH 2016

The International Training and Education Center for Health (I-TECH) is presenting three posters at the 7th Annual Consortium of Universities for Global Health (CUGH) conference in San Francisco on April 9-11. The theme of this year’s conference is “Bridging to a Sustainable Future in Global Health.”
A critical component in sustainability is the ability to collect accurate and meaningful data through electronic medical records (EMRs) – the subject of two abstracts from the I-TECH Kenya team.
In addition, online learning and electronic learning (e-learning) provides opportunities for health care workers in resource-limited settings to gain critical knowledge and skills while minimizing their need to leave the workplace.
In close partnership with the University of Washington Department of Global Health’s eLearning Initiative (eDGH), I-TECH piloted e-learning modules for KenyaEMR and transitioned the HIV management diploma program at the University of the West Indies into a blended learning program that incorporates online courses.
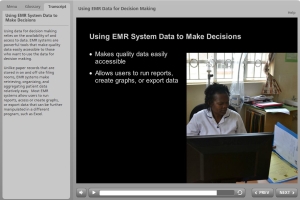
Since 2012, the Kenyan Ministry of Health, PEPFAR, and partners have supported implementation of electronic medical record systems (EMRs) at more than 600 public-sector health facilities. The International Training and Education Center for Health (I-TECH) has supported scale-up at more than 300 of these sites.
However, implementation is just part of the story. Successful, sustained use of EMR data depends upon the knowledge and skills of front-line health care workers. To address this need, I-TECH and eDGH developed and piloted two interactive e-learning modules on EMR data quality and EMR data for decision-making.
I-TECH and eDGH found that facility staff were motivated to use EMR e-learning modules and apply what they had learned. Participants found the content relevant to their jobs and cited an interest in additional scenarios and modules. Self-paced e-learning modules were determined to be a viable solution for standardizing sustainable training on EMR systems.
To support progressive EMR data quality improvement, I-TECH developed a Routine Data Quality Assessment (RDQA) standard operating procedure and analysis tool. The RDQA procedure was defined in collaboration with the Kenyan Ministry of Health and integrated within existing policies and procedures.
From 2014 to 2015, 180 baseline and repeat assessments were conducted. I-TECH supported facility personnel to share results during county-level EMR review meetings; these presentations motivated other sites to plan for RDQAs and fostered a culture of ongoing data quality improvement. The RDQA procedure for EMR data has now been institutionalized as a method for progressively improving EMR data quality in Kenya.
In partnership with the University of the West Indies (UWI), eDGH and I-TECH transitioned a one-year diploma program in the Management of HIV Infection to a blended learning platform that combines online courses with either a clinical practicum or a research project.
The shift in pedagogy, methodologies, and technologies was achieved through a three-phased approach designed to not only train UWI faculty and staff, but also transfer online facilitation skills to them and sustain those skills.
In its second year as a blended learning online program, the diploma program has scaled up to include health care workers from Cayman Islands, Jamaica, and Suriname.
These projects are supported by the Health Resources and Services Administration (HRSA) of the U.S. Department of Health and Human Services (HHS) under U91HA0680, International AIDS Education and Training Center. The content and conclusions of this post are those of the authors and should not be construed as the official position or policy of, nor should any endorsements be inferred by, HRSA, HHS, or the U.S. government.
Faculty Partnerships with University of Namibia Lead to Strengthened School of Public Health
Despite a decrease in the estimated annual HIV/AIDS incidence since 2001, HIV/AIDS remains a significant source of morbidity and mortality in Namibia.[1]
In 2008, the International Training and Education Center for Health (I-TECH) at the University of Washington (UW) was invited to conduct a rapid assessment of the University of Namibia (UNAM) master’s degree program in public health, with the goal of identifying ways to strengthen UNAM’s School of Nursing Science and Public Health. Dr. Virginia Gonzales, Senior Lecturer in the UW’s Department of Global Health and Senior Technical Specialist with I-TECH, led that study along with Lee Pyne-Mercier, UW Affiliate Instructor and former I-TECH Country Program Manager.
New award based on study findings
Recommendations included the suggestion that UNAM attract lecturers from outside the university to strengthen teaching in subjects such as research methods, epidemiology, and biostatistics. Based on these and other findings from the assessment, UNAM and UW/I-TECH submitted a joint application to the US Centers for Disease Control and Prevention (CDC) and were awarded a five-year cooperative agreement in 2010, with Dr. Ann Downer, Executive Director of I-TECH, serving as principal investigator.
The goal of the agreement was to improve and enhance the UNAM School of Nursing Science and Public Health. Objectives for this project included:
- Plan for sustainability and transfer of resources to UNAM.
- Strengthen professional development and faculty support at UNAM.
- Strengthen content and delivery of the MPH program at UNAM.
- Improve research capacity and output of lecturers and students at UNAM.
- Strengthen institutional capacity and infrastructure for teaching public health at UNAM.
With this new award, I-TECH/UW and UNAM embarked upon a series of faculty partnerships. The group also began to explore how to separate the UNAM School of Nursing Science and Public Health into two programs, creating both a School of Nursing and a School of Public Health. The UNAM Senate issued a proclamation in 2014 that this would occur.
“The focus of curriculum [in the new School of Public Health] will be needs-driven,” says Dr. Käthe Hofnie Hoëbes, Associate Dean of the UNAM School of Nursing Science and Public Health, “and it will support new job growth in Namibia, as it promotes the creation of new cadres of public health specialization.”
From partnership comes growth
The CDC award has now come to an end; however, through this project, UW and UNAM created 16 strong faculty partnerships, all determined by the priorities of the UNAM faculty through a Public Health Working Group (PHWG).
“The benefit of working with the PHWG was one of the key takeaways from this project,” says Dr. Gonzales. “It ensured that UNAM was in the position to offer continual input, guide project activities, and truly lead the project.”
The faculty partnerships occurred in health policy, bioethics, nutrition, research, environmental health, and epidemiology, linking interested faculty at UW and UNAM. Through these relationships, UW faculty visited the main UNAM campus in Windhoek to facilitate workshops and review curriculum, and the UNAM faculty visited UW to observe classes and work on curriculum revision.
As a result of the trust among faculty at both universities, partnerships evolved in unexpected areas as well, including social work, nursing, medicine, pharmacy, teaching technologies, and with the Namibian Ministry of Health and Social Services’ (MOHSS) Primary Health Care Program.
“Working in partnership was a cross fertilizing, fulfilling and enriching exercise for all of us who were involved,” says Magdaleena Nghatanga, former Director of the Directorate of Primary Health Care, MOHSS. “Across the ocean we shared experiences and professional expertise. Utilizing technology such as Skype, Dropbox, and e-learning helped the team in developing and revising the curriculum, as well as in building and improving teaching at the university level. As a result, the Primary Health Care Program and curriculum were revised and updated, and the students were thrilled with the new lectures.”
Outcomes echo throughout the country
The collaboration also focused attention on teaching skills, and evaluations of faculty by students at UNAM improved considerably. In addition, UNAM graduates reported improved skills and knowledge in HIV/AIDS, nutrition, health policy, epidimiology, and research and increased knowledge of and interest in public health. Thesis supervisors at UNAM reported greater skills in supervision and student mentoring, and UNAM lecturers reported increased knowledge, skills, and confidence in teaching course materials.[2]
The workshops offered on learning theory and teaching skills were later scaled to all of UNAM, including remote campuses. Several faculty also participated in the Leaders in Health – Namibia! (LIH) program that was designed by I-TECH/UW in collaboration with the MOHSS in order to strengthen the health care delivery system in Namibia through effective mentoring of health leaders and managers. The UNAM faculty who participated in LIH later improved course content on leadership and management at UNAM by using material and content from LIH.
“This partnership has yielded benefits on many fronts,” says Dean Hofnie Hoëbes. “Lines of collaboration have been initiated with other world-class universities, and technical support was provided for the roadmap for establishing a standalone School of Public Health. This will benefit the nation as a whole by supporting public health care in the country and preparing a larger, professional workforce with specialized skills to address shortages in public health practitioners in Namibia.”
_________________
[1] Namibia Global Health Initiative, 2011-2015/16.
[2] University of Namibia and I-TECH Namibia. Evaluation of the Impact of the UNAM/I-TECH Collaboration upon the Master of Public Health Program, 2009-2012. 2013.
Tablets Help Tanzanian Health Care Workers Upgrade Skills
In November 2014, the Tanzania Ministry of Health and Social Welfare (MOHSW) launched a program that allows practicing Clinical Assistants to upgrade to the level of Clinical Officer — the first MOHSW distance learning program in Tanzania to use tablet computers to deliver medical course material.
The International Training and Education Center for Health (I-TECH) and the University of Washington Department of Global Health’s e-learning group (eDGH) collaborated with the MOHSW on the In-Service Programme for Ordinary Diploma in Clinical Medicine, a blended distance learning program.
Credential upgrades expand the range of health care services that these practitioners can provide, including care and treatment of HIV and AIDS. They are also expected to have a positive impact on retention of healthcare workers. The use of tablet technology makes these upgrades more convenient and accessible.
“Working students need learning that will not take them off their workstations for relatively long periods of time,” says Dr. Fabian Mghanga, Principal of Mtwara Clinical Officers Training Center. “Being appropriate to their situation and context, this tablet e-learning [program] provides answers to their demands.”
Support for this project was provided through the U.S. President’s Emergency Fund for AIDS Relief (PEPFAR) by the U.S. Department of Health and Human Services’ Health Resources and Services Administration (HRSA). Programmatic oversight was provided by the U.S. Centers for Disease Control and Prevention (CDC) in Tanzania.
A comprehensive educational experience
I-TECH has worked with the MOHSW since 2010 to redesign the Clinical Officer upgrading program to align with current clinical guidelines and competency-based training approaches. Sixty-five students, based at health facilities throughout the country, have enrolled in the inaugural cohort, at three Clinical Officer Training Centers based in Kilosa, Mafinga, and Mtwara. Scale-up to additional training centers is planned for next year.
The new two-year Clinical Officer upgrading program incorporates three modalities: self-paced learning using interactive e-learning materials on tablet computers, face-to-face classroom activities and instruction, and hands-on practical training in clinical settings.
Upon completion of all course requirements, students will earn a Diploma in Clinical Medicine after achieving a passing mark on the National Qualifying Examination.
An app for self-directed learning
I-TECH and eDGH instructional designers and e-learning specialists collaborated with the MOHSW to design a digital textbook application for the Android platform. Students will complete e-learning modules using this app during self-study periods.
The app is designed to enhance self-directed learning by embedding interactive quizzes, anatomy tutorials, and other learning exercises into the course text. It also includes full-color photos and videos that are not available in the traditional residential training program.
MOHSW and training center representatives designed the course schedule and clinical rotation plan, provided clinical review, app testing, and assisted in the design of learning exercises.
“This modality of learning is quite amazing,” says Dr. Mghanga. “Our students can learn almost anything, wherever they are, at their own time and pace, yet feel they are no less [informed] than the on-campus students.”
Preparing for sustainability
In preparation for the official launch, I-TECH officially handed over all teaching and learning materials, including a donation of 73 tablet computers, to the Human Resource Development Department of the MOHSW. Tablets were distributed to students and faculty at each participating training institution.
I-TECH and the MOHSW conducted a faculty orientation to prepare principals and instructors at each training institution to successfully facilitate a distance learning program. In turn, training center faculty conducted student orientations at each site during the first face-to-face session.
In the coming weeks, the MOHSW and I-TECH will orient distance education mentors based near students’ homes, who will support students during practical rotations.
I-TECH will evaluate the first year of course implementation, and results will inform future scale-up and transition planning with the MOHSW to help ensure a sustainable program. To further support sustainability, the MOHSW has established a revolving fund to purchase tablets for future student cohorts.
E-Learning Increases Accessibility to HIV Diploma Program in the Caribbean
Students of the graduate diploma program in the management of HIV infection have the opportunity to receive instruction from a hand-selected group of experts. Photo courtesy of Ben Depp.
In the Caribbean, an estimated 250,000 people are living with HIV (UNAIDS, 2013). To address this epidemic, health workers must have the latest information to guide the treatment and care of those living with HIV and AIDS. The University of the West Indies (UWI) St. Augustine campus in Trinidad and Tobago offers a one-year graduate diploma program in the management of HIV infection.
In partnership with UWI and the Caribbean HIVAIDS Regional Training Network (CHART), the International Training and Education Center for Health (I-TECH) and University of Washington Department of Global Health’s eLearning Program (eDGH) helped to transition the program to a blended learning platform — one that offers courses online as well as an in-person practicum.
Support for this transition was provided by the U.S. President’s Emergency Plan for AIDS Relief (PEPFAR) through the Department of Health and Human Services’ Health Resources and Services Administration (HRSA).
The program recently completed its first semester in this new format. With the expanded platform, students have the flexibility to access the course material “anytime and anywhere,” says Professor Zulaika Ali, Program Coordinator, “and it allows students to organize their training around their routine activities, which is important for mature working individuals.”
The conversion of courses online creates a one-of-a-kind program in the Caribbean, increasing access for mid-career health professionals working in the public sector, for non-governmental organizations (NGOs), and for commercial organizations. The program was designed for medical doctors, pharmacists and dentists, as well as nurses with bachelor degrees from any recognized university; registered nurses with a minimum of three years of experience; social workers; management staff from government ministries, private sector and NGOs; and tutors and lecturers in training institutions.
After a week-long online student orientation, students explore the following topics through online instruction and relevant resources, synchronous virtual classroom sessions, and collaborative activities and discussions. At the end of each semester, students complete an in-person exam. After completion of the online courses, students participate in an in-person practicum or dissertation. Courses include:
- Research Methods and Design
- HIV Epidemiology and Pathogenesis
- Laboratory Techniques for Diagnosis of HIV
- General Management of HIV/AIDS
- HIV Co-Infection and Other Related Issues
- HIV Health Systems
- Sexual and Reproductive Health
In addition to the flexibility this part-time program offers, students also have the opportunity to receive instruction from a hand-selected group of experts from around the globe, including professors, health care workers from the Ministry of Health and NGOs, and professionals practicing in the region.
Transition from in-person to blended learning
In late 2013, I-TECH and eDGH were approached by UWI to convert the in-person diploma program into its second, blended rendition. The team started by piloting two courses online in the Moodle learning management system (LMS). From there, they obtained critical feedback for the remainder of the conversion.
Their research showed that students felt the course content was clear, appropriate, interesting, and applicable to their work and reported a preference for recorded lectures and relevant videos, anytime/anywhere access, and interactions with instructors and peers. Likewise, faculty enjoyed building new skills through online instruction.
“We conducted two in person, on-site faculty workshops, countless Skype calls, online trainings, and emails to build the capacity of faculty to develop and teach online,” says Elizabeth Scott, Senior E-Learning Developer with eDGH. “Working with faculty was a highly rewarding experience. They were motivated and dedicated, and they worked tirelessly side-by-side with us to create the best possible experience for students.”
As part of the project, the I-TECH/eDGH team also developed a commercial for the program (see below), as well as a number of introductory materials that can be used for a variety of online and blended learning programs. Among them are a general student orientation to help learners identify skills and characteristics necessary for success in online courses and an e-learning basics module for instructors.
“The informational materials developed for the program will help to improve the delivery of health care more generally,” says Dr. Ali.
A robust transition guidebook was also assembled, containing roles and expectations, best practices, online orientation materials, processes, budgeting templates, evaluation tools, job aids, and tasks and timelines for faculty and staff for ease of handover from year to year.
“The delivery of this program in the blended format will have a tremendous impact on the quality of care delivered to people infected with and affected by HIV,” says Dr. Ali. “The Faculty of Medical Sciences looks forward to welcoming regional and international students into the program. This new platform will surely enrich the learning experience of all involved.”
I-TECH Presents at CUGH 2014
I-TECH staff will head to Washington, D.C., this week to the Fifth Annual Consortium of Universities for Global Health (CUGH) Conference, which will take place at the Washington Hilton from May 10-12. More than 1,300 participants from 50 countries are expected to attend the conference, co-hosted by the George Washington University and Stanford University.
This year’s theme is “Universities 2.0: Advancing Global Health in the Post-MDG Era,” and I-TECH teams will present on forward-looking topics ranging from the implementation of electronic medical records to partnership with the U.S. President’s Emergency Plan for AIDS Relief (PEPFAR).
Confirmed speakers include President of the World Bank Jim Kim; former Head of UNAIDS and current Director of the London School of Hygiene and Tropical Medicine Peter Piot; and Head of the Earth Institute at Columbia University Jeff Sachs. Dr. King Holmes, I-TECH Principal Investigator and 2013 Gairdner Global Health Awardee, will also speak at CUGH’s Gairdner Lecture on May 12.
For those planning to attend the conference, don’t forget to check out the University of Washington Department of Global Health table — and to stop by the I-TECH presentations, listed below.
Kenya
- Electronic Medical Record (EMR) Implementation at Scale in the Public Health Sector: Lessons Learned in Kenya
Haiti
- Using an electronic medical record system to identify factors associated with attrition from the HIV antiretroviral therapy program at two hospitals in Haiti
- Before and After the Earthquake: A Case Study of Attrition from the HIV Antiretroviral Therapy Program in Haiti
South Africa
- Successes and challenges in liaising with PEPFAR partners and stakeholders in the TB/HIV Management Program
- Evaluation of a comprehensive HIV prevention program in North West Province, South Africa: results from the pilot
- Integrating research into program design: Conducting a situational analysis to inform comprehensive HIV prevention and care in North West Province, South Africa
- Mystery patients: Training actors to serve as unannounced standardized patients to evaluate training outcomes for sexually transmitted infections in South Africa
Lab Leadership and Management
- Certificate Program in Clinical and Public Health Laboratory Leadership and Management
Contact Anne Fox in Communications to see any of these completed posters.
About CUGH:
Founded by leading North American university global health programs, CUGH aims to:
- Define the field and discipline of global health;
- Standardize required curricula and competencies for global health;
- Define criteria and conditions for student and faculty field placements in host institutions;
- Provide coordination of projects and initiatives among and between resource-rich universities and less-developed nations and their institutions.
CUGH is dedicated to creating balance in resources and in the exchange of students and faculty between institutions in rich and poor countries, recognizing the importance of equal partnership between the academic institutions in developing nations and their resource-rich counterparts in the planning, implementation, management and impact evaluation of joint projects.
The Bill & Melinda Gates Foundation provided the leadership and funding to plan this consortium. The Rockefeller Foundation provided a grant to help develop the organizational structure of CUGH in its first year of existence.
Launch of HIV Programs in Zimbabwe Hits the Right Note
To the brass beats of the Prince Edward School Jazz Band, on Feb. 6, a crowd of approximately 150 government officials, health professionals, and members of the press celebrated the launch of three programs in Zimbabwe, two of which are implemented by I-TECH Zimbabwe and partners. These vital programs aim to build local capacity and provide comprehensive services to prevent and combat HIV/AIDS in the country.
Speaking at the festivities were David Bruce Wharton, U.S. Ambassador to the Republic of Zimbabwe; Dr. Owen Mugurungi, director of the AIDS and TB Unit at the Ministry of Health and Child Care (MOHCC); Dr. King Holmes, Chair of the Department of Global Health at the University of Washington; Dr. Ann Downer, Executive Director of the International Training and Education Center for Health (I-TECH); and Dr. Batsirai Makunike-Chikwinya, Country Director of I-TECH Zimbabwe.
“Preventing the spread of HIV/AIDS is important to all of us, as is providing the best level of care to those living with this disease,” said Amb. Wharton. “Today we celebrate the launch of programs that will help us reach these goals together – programs that were designed together, by dedicated teams of collaborating partners from Zimbabwe and from the United States.”
In this spirit of collaboration, the programs, totaling $65 million over five years, support the Zimbabwe MOHCC with grant funding by the U.S. President’s Emergency Plan for AIDS Relief (PEPFAR), technical support from the Centers for Disease Control and Prevention, and implementation by local and U.S.-based partners. These partners include I-TECH; Zimbabwe Association of Church-Related Hospitals; Zimbabwe Community Health Intervention Research Project; Compre Health Services; The Newlands Clinic and Newlands Clinic Training Centre; Pangaea Global AIDS Foundation, Zimbabwe; and the University of Zimbabwe-University of California, San Francisco Collaborative Research Programme.
The Training and Mentoring Program seeks to develop and deliver in-service training on antiretroviral therapy, including the medical management of HIV/AIDS, women’s reproductive health, tuberculosis (TB), and TB/HIV co-infection to 8,000 health care workers across the country over five years. A mentorship component will also provide health care workers with access to ongoing learning and feedback on clinical issues. Health workers will receive refresher trainings via distance learning technologies, and the effectiveness of the program will be measured through a training database.
Also celebrated – and accompanied by a ribbon-cutting and presentation of 17 new vehicles – was the launch of the Voluntary Medical Male Circumcision Program. The program, building on work that started last spring, seeks to deliver services to 412,000 men in Zimbabwe between the ages of 15 and 49 years over the next five years. Medical male circumcision has proved very effective in preventing the spread of HIV. Randomized controlled trials in Uganda, Kenya, and South Africa have shown that this intervention reduces the risk of female-to-male sexual transmission of HIV by approximately 60%.
“Together, these two programs will improve the effectiveness and quality of prevention, treatment, and care services for those affected by HIV/AIDS – and create better health systems for all Zimbabweans,” said Dr. Holmes.