The global health community recognizes March 24 as World Tuberculosis (TB) Day to raise awareness of this deadly, yet preventable and curable, disease. The 2021 theme, “The Clock Is Ticking,” underlines the importance of acting now to end the global TB epidemic. According to World Health Organization, the probability of developing active TB disease is 18 times higher in people living with HIV (PLHIV), and in 2019 TB killed 1.4 million people worldwide, which includes 208,000 people who were HIV-positive.

According to the U.S. Centers for Disease Control and Prevention, TB is one of the leading causes of death worldwide for PLHIV. To help treat and combat the spread of TB, particularly among PLHIV, the International Training and Education Center for Health (I-TECH) supports TB prevention, care, treatment, monitoring, and policy activities across the I-TECH global network. Current I-TECH work includes TB interventions in Mozambique, Namibia, and Malawi.
I-TECH supports the National TB Program in Mozambique by using the Warm Line—a telephone consultation line that supports clinicians—to deliver results for suspected drug-resistant TB cases to clinicians located at health facilities throughout the country. This collaboration with the Ministry of Health’s National TB Reference Lab allows for more timely identification and better management of drug-resistant TB cases. During 2019, 9,103 (83%) of results were delivered via the Warm Line. I-TECH’s team also engaged providers and clinicians in 383 interactions via the Warm Line to support mentoring and to monitoring complicated TB cases.
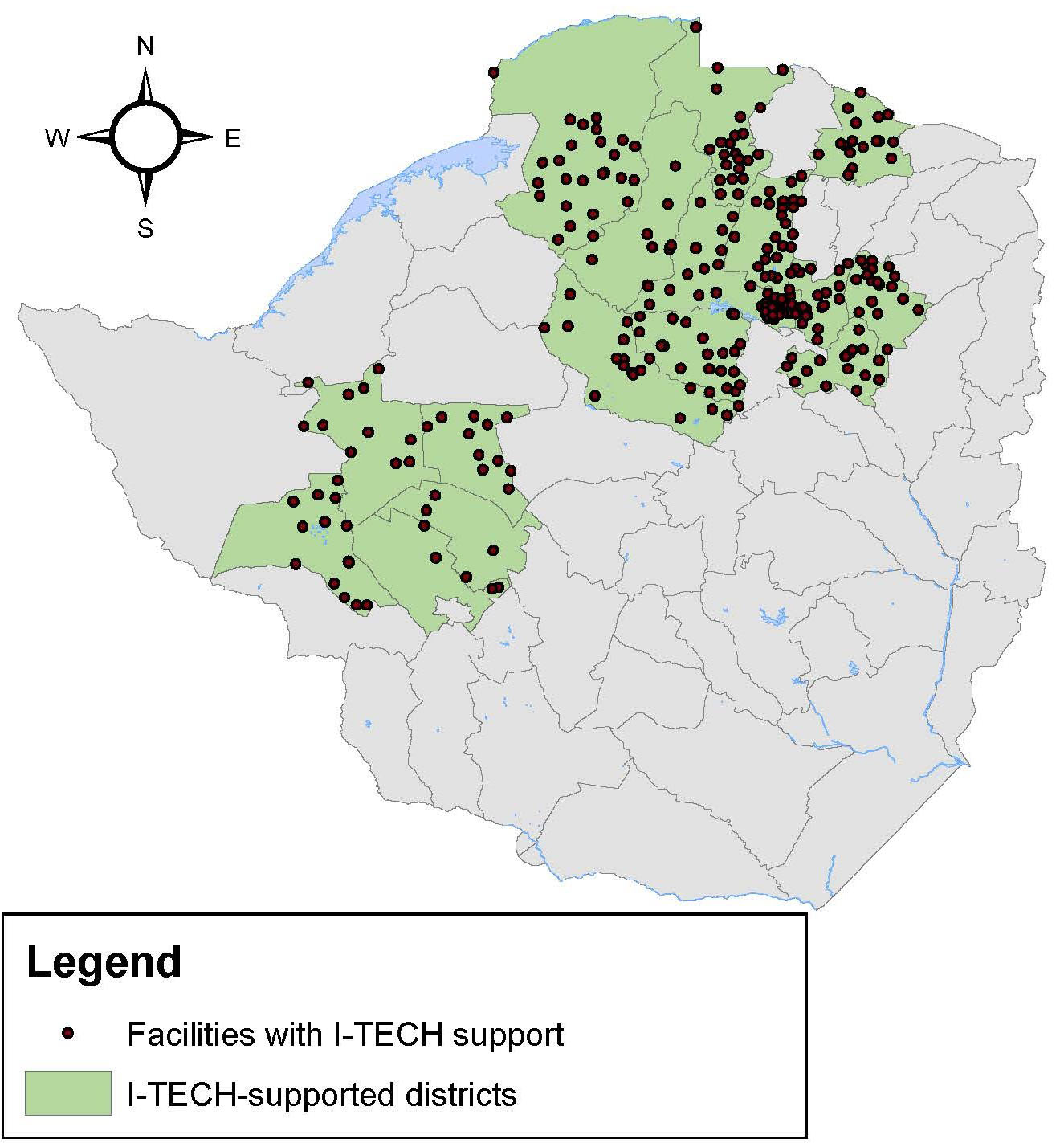
In addition to supporting clinicians with TB care and diagnosis, I-TECH supports TB prevention, diagnosis, and care among clients attending HIV clinics throughout seven regions and across 150 public health facilities in Namibia. The I-TECH team screens for active TB; monitors drug interactions for TB/HIV co-infection; provides TB screening, prevention, and management of TB/HIV co-infection for HIV-positive clients; tests for HIV at TB clinics for clients with unknown HIV status; and assesses eligibility, previous initiation, and completion of TB Preventive Therapy (TPT) to ensure no clients are missed. As of January 2021, approximately 90% of HIV-positive patients on antiretroviral therapy at supported facilities initiated their TPT course and 80% have completed their TPT course. I-TECH also works closely with healthcare workers and facilities to improve recording keeping of TPT course initiation and completion as well as the use of this data to focus day-to-day clinical efforts.
Since 2015, I-TECH has been providing technical assistance support to the Malawi National TB Program to improve the quality of TB services at all health facilities throughout Malawi. I-TECH continues to train program monitors to interpret and act on data collected using the TB Standard of Care Monitoring Tool. The tool, designed by I-TECH, collects data for case detection, treatment outcome monitoring, TB/HIV status ascertainment, and TB infection control and contact investigation. Using the collected data, I-TECH identifies performance gaps and create action plans for health facilities to improve the quality of TB services. Even with a loss of momentum due to the impact of COVID-19 pandemic, by September 2020, 85% of presumptive TB cases—those who were suspected of TB and referred for testing—knew their HIV status.
I-TECH’S WORK IN MOZAMBIQUE IS SUPPORTED BY THE HEALTH RESOURCES AND SERVICES ADMINISTRATION (HRSA) OF THE U.S. DEPARTMENT OF HEALTH AND HUMAN SERVICES (HHS) UNDER U91HA06801, THE INTERNATIONAL AIDS EDUCATION AND TRAINING CENTER (IAETC). THE CONTENT OF THIS POST IS THE AUTHOR’S AND SHOULD NOT BE CONSTRUED AS THE OFFICIAL POSITION OR POLICY OF, NOR SHOULD ANY ENDORSEMENTS BE INFERRED BY HRSA, HHS OR THE U.S. GOVERNMENT.